When Is Open Enrollment for Health Insurance in 2025?
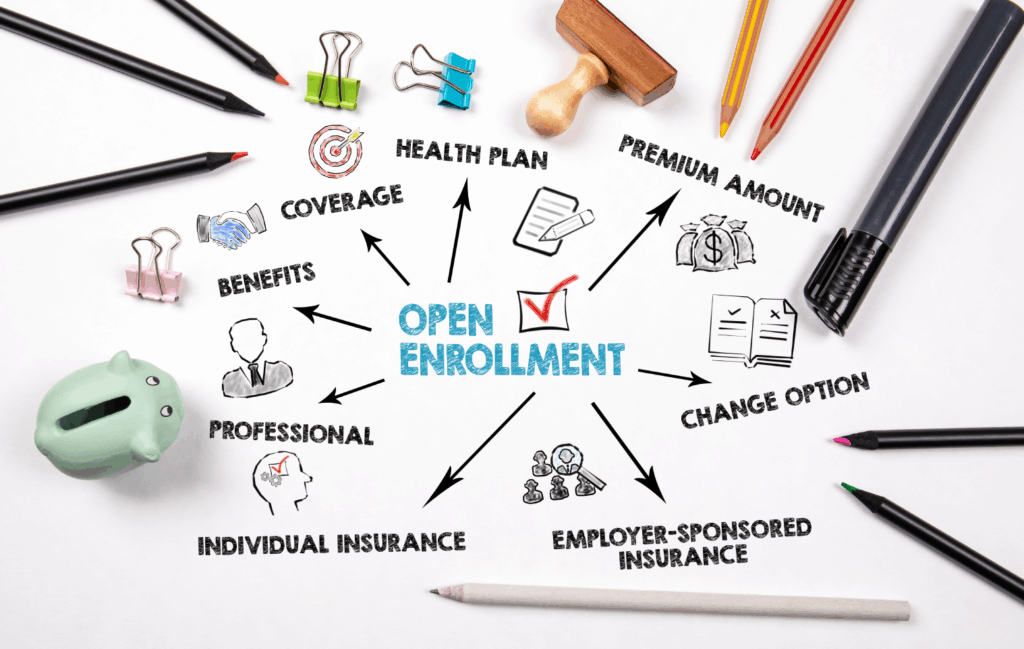
If you’re considering health coverage for year 2025, or planning ahead for year 2026, one of the the most important windows of time to mark on your calendar is the open enrollment period. This is the period when individuals, families, and employers may enroll in or change their health insurance plans without requiring a “special qualifying event”. If you miss this window of time, you may end up stuck waiting until next year, unless you do qualify for a special enrollment period.
Here at The Lambert Agency, we’re able to help employers and employees understand all associated timelines and ensure nobody ends up missing out on their chance to secure coverage they need. Here’s what you need to know.
Important Dates for 2025 / 2026 Coverage
Marketplace (ACA / Exchange) Plans
For many states using the federal Health Insurance Marketplace (Healthcare.gov), here are the key dates to mark on your calendar:
- Open Enrollment begins: November 1, 2025 (HealthCare.gov)
- Deadlines for January 1, 2026 coverage:
• December 15, 2025 — last day to enroll or change plans if you want coverage to start January 1. (HealthCare.gov) - Open Enrollment ends: January 15, 2026 (HealthCare.gov)
- If you enroll between December 16, 2025 and January 15, 2026, your coverage typically begins February 1, 2026 (HealthCare.gov)
Note: some states may run their own exchanges and may have different open enrollment windows (for instance, California’s ends January 31). (HealthMarkets)
Employer-Sponsored Health Insurance
If you healthcare coverage does come through your employer, your employer is the one who set the open enrollment dates, most commonly set sometimes in the fall season. Many companies will end up running open enrollment in the months of October or November, allowing coverage to begin on January 1st of the following year. (Fidelity)
For this reason, it’s critical for HR or benefits teams to fully communicate those dates clearly, as missing these specifics dates means the employees may not be able to make changes to their health insurance coverage outside of special qualifying events (unless permitted otherwise under said plan).
Special Enrollment Period (SEP)
Outside of the open enrollment window, one may still qualify to enroll or make changes if they experience a qualifying life event, such as:
- Losing existing coverage (e.g. job-based plan ends)
- Marriage, divorce, or legal separation
- Addition of a child (birth, adoption, etc.)
- Moving to a new area
- Other events defined by the marketplace or your plan
These events will often trigger a 60-day window (before or after the event) to enroll via a SEP. (healthinsurance.org)
How Missing Open Enrollment Matters
- If you don’t enroll during the open enrollment period or make changes during the open enrollment period and you do not qualify for SEP, you’ll likely have to wait until the next open enrollment period the following year. (healthinsurance.org)
- For the healthcare marketplace, if you miss the December 15th deadline for January coverage, you may still enroll prior to January 15th, yet your plan will kick in on February 1st instead. (Centers for Medicare & Medicaid Services)
- Automatically re-enrolling into your last year’s plan is common; however, it may not be optimal, especially if your health situation or costs have moderately or drastically changed. (Centers for Medicare & Medicaid Services)
Tips to Prepare (For Employers & Employees)
- Communicate early & often
Begin to inform employees well in advance of the open enrollment period. It’s a good idea to utilize multiple channels to communicate these notices, such as email, meetings, text reminders, or printed guides placed around the office. - Offer decision support
Provide employees with benefits guides, side-by-side comparisons, and ample opportunities to ask any and all questions they may have. Additionally, one-on-one sessions will likely help. - Highlight deadlines clearly
Truly emphasize the December 15th deadline (for January 1st) and the January 15th deadline, and clarify the implications of enrolling post December 15th (i.e.: a February start date of coverage). - Encourage review, not just passive renewal
Even if someone happens to be auto-enrolled, you should still encourage them to review their plan options. This is especially true if their healthcare needs or finances have changed over the past year. - Train managers & HR teams
Ensure your internal management or HR team understands how the Marketplace plans and SEPs work so they can best inform employees.
Sample Timeline (2025–2026)
| Date | Event |
|---|---|
| Nov 1, 2025 | Marketplace open enrollment opens |
| Dec 15, 2025 | Last day to enroll/change for Jan 1 coverage* |
| Jan 1, 2026 | Coverage begins for those who enrolled by Dec 15 |
| Jan 15, 2026 | Open enrollment ends; last chance to enroll/change for Feb 1 coverage |
| Feb 1, 2026 | Coverage begins for those enrolling between Dec 16 and Jan 15 |
* If you enroll after Dec 15 (but on or before Jan 15), your coverage generally starts Feb 1. (HealthCare.gov)
Contact The Lambert Agency Today for Your Open Enrollment Needs
Open enrollment is the annual window of time which bridges one health plan year to the next. For marketplace (ACA) plans, the primary period runs November 1, 2025 through January 15, 2026 in most states. Employer plans will have their own dates, typically running during the fall.
Here at The Lambert Agency, we’ve been able to help many employers navigate these open enrollment timelines, design and implement smooth enrollment processes, and communicate benefits in a concise and simplified way to drive engagement and utilization. If you’d like help preparing your organization for 2025 open enrollment (or 2026), we’re here to help every step of the way!